Tools and checklists
Overview of all Tools and Checklists recommended in this Guide
Planning, recruiting, engagement and investment...
From recommended contributors to communicating with patients throughout...
Identify and engage with stakeholders to ensure...
Although you may not have selected the expert patients or patient groups...
This charter is designed for open communication with all potential Patient Advisory Board...
HollandBIO and admedicum asked Marleen Katee and Maryze Sconeveld van der Linde...
Following a general understanding of the patient journey and unmet needs...
There are many ways to identify patients to be involved in an interaction...
The four key principles for collaboration...
Patients, patient representatives and industry should take responsibility to ensure...
Clinical trial stakeholders include not only the potential participants you hope to enroll...
This list of questions is non-exhaustive but may help with making a strong start...
Help us improve this guide
Submit Feedback
Checklist
Preparing a collaboration
Defining the interaction
Patients, patient representatives and industry should take responsibility to ensure interactions are meaningful by clearly defined processes and actions, progressed to timelines. In addition, all participants should be prepared for the interaction.
Prior to each interaction, agree mutually on (where applicable):
- The objective of project involving patients and/or areas of common interest to establish agreed structured interaction, providing all parties with necessary protection with regards to independence, privacy, confidentiality and expectations (see section 11. written agreement)
- The type of input and mandate of the involved person
- The tools and methods of interaction, e.g. types and frequency of meetings, ground rules, conflict resolution, evaluation
- Desired patient / patient partner organisation to foster long-term working partnerships, with independence ensured (in scope)
- The profile of the type of patient/s or patient representatives/s to be involved and their number
- How activity outputs will be used and ownership of outputs
- How and when the patient/s involved will be informed of outcomes
- Contractual terms and conditions including consent and compensation (see section 11, written agreement).
- Other elements according to the specific project
Source
Download
Checklist
Preparing a collaboration
The four key principles for collaboration:
1. Clarity of Purpose
Each party should be clear about the reason for and the planned outcome of the collaboration – and the ultimate benefit for patients
2. Integrity
Each party should act and be seen to act honestly and with integrity at all times
3. Independence
Each party should maintain their independence
4. Transparency
Each party should be open and honest about the purpose of the collaboration and be able to account publicly for the associated activities and any exchanges of funding
Using this guide: a checklist
- Has there been a frank discussion about the purpose and expected benefits of the collaboration, and any risks, addressing all the issues in this guide?
- Are the objectives and planned outcomes of the collaboration specified?
- Are the roles of each partner and reporting mechanisms specified?
- Has a written agreement or contract been put in place, which sets out how each party will adhere to the four key principles?
- Is there a named senior individual accountable for managing and maintaining the relationship and monitoring adherence to the four key principles?
- Is information about the collaboration published on the company and charity websites?
- Can each party confidently explain the collaboration in public?
Source: National Voices, The Association of the British Pharmaceutical Industry (ABPI) (2015): Working
Download
Tool
List of useful conferences
Important international multi-stakeholder conferences with patient advocates included
ECRD: European Conference on Rare Diseases and Orphan Products
Rare diseases conferences (focus industry) with patient advocates included
The Global Orphand Drug Conference and Expo
You may be want to attend conferences from patient groups to learn from their interactions and subjects about their needs. Many of these conferences are open for industry participants but one should keep in mind that these events are from patients for patients and industry should respect the guest status.
Example for an indication specific conference by and for patients (industry welcome)
European Rett Syndrome Congress (international)
Also many patient organizations welcome industry at their charity events as a sponsor and as participants, like at charity runs. Check out your area of engagement.
Checklist
Mapping the Patient Landscape
Following a general understanding of the patient journey and unmet needs and before systematically interacting with patients and KOLs in a specific therapeutic area a company should have an understanding of the stakeholder field. The checklist below can help you obtain such an understanding, by:
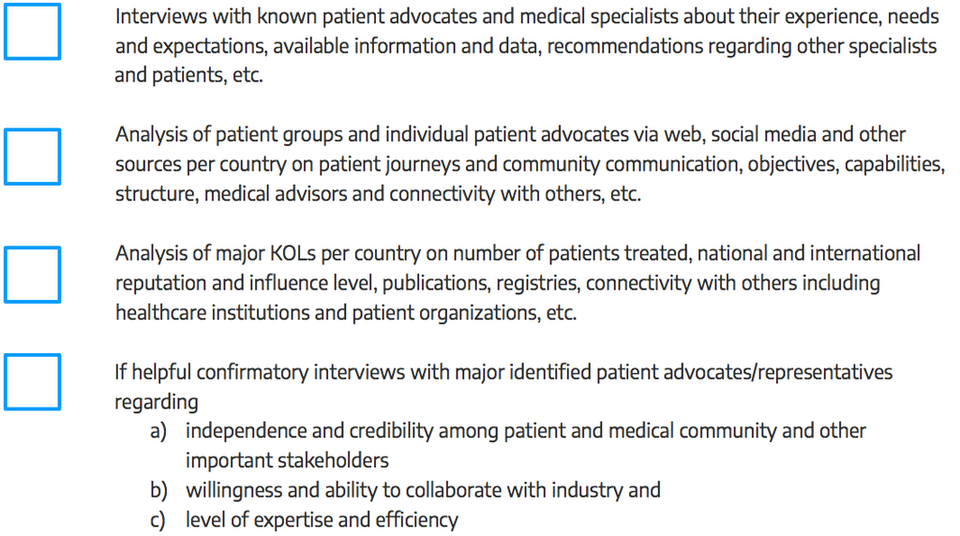
Source: This checklist has been developed by admedicum® Business for Patients GmbH.
Download
Checklist
Patient identification
There are many ways to identify patients to be involved in an interaction. The main routes are through:
- Existing patient organizations
- EUPATI or similar project
- Advertising opportunities for patient participation
- Medical Key Opinion Leaders. healthcare providers, hospitals and researchers and other institutions
- Systematic social media search for patient exchange platforms
- Unsolicited requests previously made by interested parties
- Existing advisory boards / groups (e.g. EFPIA Think Tank, Patients and Consumers Working Party at the EMA)
- Specialized patient engagement agencies
Source: European Patients’Academy on Therapeutic Innovation (EUPATI) (2016): Guidance for patient involvement for industry-led medicines R&D. (12/06/17)
Download
Tool
Defining the Patient’s Role
Although you may not have selected the expert patients or patient groups (EP/PGs) yet, outlining their roles and responsibilities at this stage helps to define your needs. Keep in mind that EP/PG roles may vary at different stages of the program or may evolve in response to new requirements. Once selected, discuss the roles with your EP/PGs to clarify what they can contribute based on their unique expertise and experience and avoid misunderstandings at the outset, e.g. if they’re expecting to have a partnership role but you’ve designed reactor role (see Types of Patient Roles chart below).
| Patient role | Examples | Engagement level |
| Partnership role |
| High |
| Advisor role |
| Moderate |
| Reactor role |
| Low |
| Trial or study participant |
| None |
Source: DIA (2017): Considerations Guide to Implementing Patient-Centric Initiatives in Health Care Product
Development. (02/06/17)
Download
TOOL
Feedback of a Patient Organization
HollandBIO and admedicum asked Marleen Katee, President of PSC Patients Europe, and Maryze Sconeveld van der Linde, Patient Advocate Pompe Disease, the following questions:
“What is most important to you when working with the industry?”
- Relationships are built on trust. A “warm” (personal, trustworthy, sustainable) relationship is the best way forward, especially in long-lasting collaborations.
- Work with us. Patient experts are patients themselves, so we have different needs and priorities than healthy individuals. For example: we aren’t deadline junkies. Give us at least 3 weeks to get back with an answer.
- Be clear on what the (mutual) expectations are.
- Do not only talk to us, but above all listen to us. Amazing things can happen…
- Please don’t ask us to translate: we are not a translation agency, we are a patient organization!
“What does the industry need to consider when collaborating with patients / patient organizations?”
- Create lay versions of every paper/document you publish or use, including Travel Policies, Informed Consent and Data Privacy documents.
- Work with the patient organizations on those lay versions. With all due respect, as researcher it might be a bit of a challenge to figure out if a text is well-understood or not. This is your ultimate opportunity to give back to the community!
- Train your researchers, event managers, legal counsels etc. on patient-related matters, including how to embed the patient’s voice in your research. Make sure they see the benefits of patient involvement, instead of it being an obligation. Learn them to talk with patients as an equal partner. Above all, learn clinicians & researchers to listen to the patients.
- Don’t expect the patient (or patient organization) to do all kind of things free of charge. You don’t do that either, do you? A fee is great. However, some patient experts cannot accept a fee, as that will have a huge (negative) influence on their finances (e.g. on welfare or on disability leave) . You can offer to donate to a charity of their choice. Solved!
- Accommodate patients needs: if there is a visit, make sure there is wheelchair access, a meal matching our dietary needs. If we need to come a day earlier because we are tired, so be it. Don’t discuss, just do it and make it happen.
- Expect patients to need more extended deadlines. Being ill is a fulltime job already.
Source: This tool has been developed by admedicum® Business for Patients GmbH.
Download
Tool
Considerations for Implementing Expert Patient or Patient Group Input
Recommended contributors :
- Program leaders
- Patient liaisons
- Sponsor representatives
- Clinical investigators
- Research team
- Trial site staff
- IRB
- Expert patient(s)/patient group representatives
Communicating with patients throughout the program
- How does the phase of drug/biologic/device development process covered by this program impact communication with patients?
- What translation and/or cultural adaptions are necessary?
- Wat language will be used to communicate with and about the patients?
- Are research questions and procedures culturally sensitive and appropriate?
- How will patients be referred to (e.g. “subject” vs. “patient” vs. “participant”)?
- What is the communication plan for patients throughout the program?
- Message content
- Audience
- Messenger
- Delivery mechanisms
- Timing
- Feedback mechanisms
- What feedback mechanisms and processes are in place for the patients to comment on sites, investigators, and the study participant experience?
- What role will social media play in the communications?
- How is social media defined?
- How can social media be utilized (e.g. for trial recruitment, to educate patients)?
- What restrictions should there be, if any? Why?
- How will those limits be communicated and enforced?
- What methods will be used to interact with patients and other stakeholders?
- Focus groups
- Interviews
- Surveys
- Inclusion in advisory councils
- Inclusion in meetings with researchers
- What data/information can and will be shared with the patients and when?
- Aggregate (de-identified)
- Patient-specific
- What are the restrictions (propieratry and regulatory) constraining the release of data?
- How do we ensure that this information is shared in patient-friendly language? How will that be determined/monitored?
Additional resources
Communication Handbook for Clinical Trials.
Guidance for Biomedical HIV Prevention Trials, p 37-38: “Stakeholder education plan.”
Download
TOOL
Building an Advisory Board
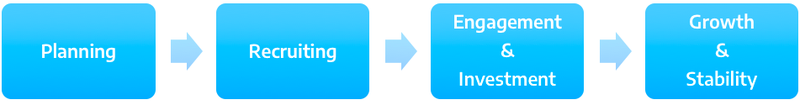
Planning
- Identify need for Patient Advisory Board
- Clarify goals of Patient Advisory Board
- Identify staff in charge of the Board
- Create vision, mission, statement
- Make logistic arrangements for Board meeting
- How long?
- How often?
- How many people?
- What incentives can be provided?
- How to proceed with travel cost reimbursement?
Recruitment
- Roll out recruitment plan
- Outreach to potential advisors
- Spread the word internally about the role of Patient Advisory Board and its importance
Engagement & Investment
- Orientation
- Goals
- Role
- Expectations
- Rules
- Establish relationship with new advisors
Growth & Sustainability
- Create a system to continue building relationships with patients
- Create a framework of regular meetings
- Maintain communication with patients, staff and leadership: develop a continuing communication system
- Explore opportunities for partnerships and growth
- Track and share successes
- Evaluate challenges and move towards solutions
Source: Modification of a toolkit for building an advisory board in hospital setting. Angel, L. (2014): Starting and sustaining a Patient Advisory Board. Patient Liaison Handbook. Family Health Center-San Francisco General Hospital. UCSF-Family Community Medicine. Source: https://www.pcpcc.org/resource/starting-and-sustaining-patient-advisory-board (02/06/17)
Download
TOOL
10 Questions for Building a Patient Advisory Board
This list of questions is non-exhaustive but may help with making a strong start. We recommend to discuss these questions with internal and external people you trust and may want to have on board.
- Why do you want to set up a Patient Advisory Board? Define a mission statement.
- What are the specific objectives and the anticipated outputs?
- Are you willing to share these objectives, critically discuss and openly communicate them to all prospective board members? (If not, this may be prohibitive for setting up such a board.)
- If confidentiality of content is required, how are you going to provide for it? E.g. will participants have to sign a Confidential Disclosure Agreement (CDA) prior to working with you? What does that mean to the process and the selection of candidates?
- How often do you think the Patient Advisory Board needs to meet and how much time should the patient advisor and your organization dedicate to the Patient Advisory Board? Is that realistic?
- Do you have your management’s support for working with the Patient Advisory Board and for spending the time, resources and money on such an effort?
- What are the skills/profiles of the participating patient experts you want as advisors?
- Who should participate in the Patient Advisory Board meeting(s)?
- Who will chair the Patient Advisory Board and who's in charge of the follow-up? Will you need an external facilitator?
- How will the logistics, compensation and legal compliance be provided for, including contractual arrangements? As you are working with patients, facilities may need to be adapted.
For more general guidance and detailed questions have a look at these sources:
EFPIA Guide “Working Together with Patient-Groups”
D.I.A. ConsiderationsGuide to Implementing Patient-Centric Initiatives
Download
Draft Charter for a Patient Advisory Board
This charter is designed for open communication with all potential Patient Advisory Board members inside and outside your organization and any other party interested in the purpose of the Patient Advisory Board and the nature of the attendees. Please note that Transparency Codes apply.
We strongly recommend to use this only as a proposal for clarifying your own thinking first and then ask all other involved stakeholders (patient experts, Key Opinion Leaders, others) to comment and add as appropriate. You may even start with an open discussion before drafting with some of the potential advisors you know you want to have on the board. The final charter should be the reflection of the major points agreed upon between the collaborators about why to collaborate on what and how to do that.
Purpose, mission and objectives
The “insert Name of the Board” shall contribute to (specify)…
- Describe what your company is currently doing, why this requires patient advice and what you hope to achieve from it.
- Describe the specific objectives the Board should strive to achieve in as much detail as possible (“to learn / get insight / discuss…”). Try to put yourself into the shoes of the potential Patient Advisory Board member reading this who will decide whether to join or not based on this charter.
- Input from (already) appointed members of the board, both inside and outside your organization, is valuable to improve the charter.
Members and responsibilities
The (insert Name of the Board) consists of (specify)…
Describe the desired profile of the external and internal board members and their expected roles:
- Who should chair the Board? Is an independent, external chair required? And what are this person’s responsibilities:
The Board will be chaired by (insert name and function). The chairperson is responsible for preparation of the meeting, including drafting the agenda and sending it to the Board for input, finalizing the agenda, moderation of the meeting itself, drafting the meeting minutes and follow-up.
- Describe the patient advisors on the board and their roles, names and backgrounds/functions:
There will be 4 patient advisors on the board:- a patient advocate on behalf of patient organization A
- a patient advocate on behalf of patient organization B
- 2 patients diagnosed with (specify indication), who have experience with (specify, e.g. specific treatment, a specific patient support program or more general “clinical development in disease X”)
- Describe the employees of your organization who should be on the board and their expected roles, names and functions:
There will be (number) company representatives on the board:- The head of clinical development
- The international project lead
- The head of market access
- etc.
- Describe any other external advisors you may want to have on your board and their expected roles:
- A physician
- An experienced patient nurse
- A social worker
- A caretaker
- etc.
Organization and logistics of the Patient Advisory Board
The “insert Name of the Board” will meet (specify)…
- Describe in detail the frequency of meetings, whether they are in person or via phone/web conference, the duration and location.
- Clarify whether confidentiality agreements are in place and provide for the board members’ freedom to communicate about the confidential information between each other:
The Board meetings will be subject to confidentiality as agreed individually in written form between the company and the board members.
- Make sure provisions are taken to ensure all Board members “speak the same language”, hereby taking into account not everyone may be fluent in English and avoiding misinterpretations. Also, local Boards can be in a different language:
All Board materials and the board meetings will be in English language. Where needed translation of materials and during meetings will be provided for.
- Make sure all participants agree on time needed for preparation:
Board members shall prepare for the board meetings based on the material provided by the Chair, which shall not exceed more than (…specify estimated time…) per board session.
- Provide for detailed loops before, during and after each session regarding possibly required adaptations.
Source: This charter has been developed by admedicum® Business for Patients GmbH
Download